
You have surely heard the terms “in-network” and “out-of-network” when referring to doctors or care facilities and your insurance plan. It can be confusing and make you wonder why it matters to you, as the consumer. Let’s explore these terms and find out more!
What are Health Insurance Plan Networks?
Health insurance plans create networks of doctors and facilities with which they have contracted to accept negotiated rates for the services they provide. When you subscribe to a specific insurance plan, you can look up the list of these contracted providers to see which ones are “in-network.” Most plans have helpful search tools online like “Find a Doctor” to save you time as you look for your specific doctor. You can also call the facility or healthcare provider and ask if they are considered “in-network” or “out-of-network” for your particular health insurance plan.
Why Choose “In-network” Providers?
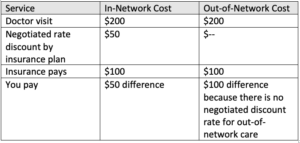
When you make the choice to see an “in-network” healthcare provider or visit an “in-network” facility, you will typically pay less for the service (doctor visit, screening, hospital stay, etc.) than if you chose to use a provider outside of the plan’s network. Your insurance plan has negotiated a discounted cost for the service and passes that savings on to you, the subscriber. See the table below for an example.
Additional Benefit to “In-Network” Care
Some health insurance plans allow you to visit “out-of-network” doctors and facilities with the understanding that you will pay more for these services since they are not in an agreement with one another. However, you may not be able to apply these expenses towards your annual deductible. This means it may take you longer in the year, with more out-of-pocket expenses, to reach your deductible. Staying “in-network” alleviates this delay and any added costs.
Staying with “in-network” providers truly equals greater cost-savings to the consumer. By doing a little research upfront to find the doctors and facilities in your plan network, you will end up with less out-of-pocket expenses for your health care each year. While the choice is ultimately up to you on who you see for your care, looking within your plan network will reap you great benefits.




